Despite 30 years of IVF practice, the process of freezing human embryos, known as vitrification, has remained extremely manual and susceptible to errors and inconsistencies by embryologists. In 2009, Genea Biomedx teamed up with Planet Innovation to solve this challenge by automating IVF vitrification and finally making the process consistent and standardized for labs around the world.
Despite 30 years of IVF practice, the process of freezing human embryos, known as vitrification, has remained extremely manual and susceptible to errors and inconsistencies by embryologists. In 2009, Genea Biomedx teamed up with Planet Innovation to solve this challenge by automating IVF vitrification and finally making the process consistent and standardized for labs around the world.
The fragile nature of human embryos made automation a massive challenge
There are approximately 1.5 million assisted reproductive cycles, such as IVF, in the world each year. Embryos which are not transferred immediately back to the mother during the initial IVF cycle are placed in cryo storage, through a process called vitrification, for use in later cycles. This process has remained manual due to the extremely complex and fragile nature of embryos, which makes handling them through automation incredibly difficult. The problem with this current manual process is that it requires an embryologist to sit there for a considerable amount of time handling the embryo. This can introduce inconsistencies in the handling of each embryo which in turn can reduce the rate of successful embryo recovery. The existing process also places the human embryos directly in contact with liquid nitrogen which introduces a risk, albeit very small, of contamination.
In 2009, Genea Biomedx teamed up with Planet Innovation to try to automate IVF vitrification and finally make the process consistent and standardized. The ‘big idea’ was to locate the embryo safely and bring all the required fluids to the embryo – instead of moving the embryo from fluid to fluid as was the case in the traditional manual process. To achieve this, a lot of obstacles had to be overcome.
Vitrification is highly specialized. About half the world’s IVF labs don’t do it, although they would like to if they could. For the countries that do use vitrification there are a range of issues that can lead to embryo loss. To ensure we fully understood the problem before we dived into solution mode, we conducted voice-of-customer studies involving respondents from around the world. What we found was that all countries loved the idea of automated vitrification but for different reasons depending on the nature of their IVF industry.
Voice of customer revealed hidden requirements by regulatory authorities
During the voice-of-customer studies we also found that the various regulatory authorities wanted the frozen embryo physically separated from the liquid nitrogen – a request that had not initially been predicted. The reason for this request was that scientific literature had revealed that HIV and other viruses could live at -190 degrees Celsius and could theoretically infect an embryo. Although this had never been known to have happened, to satisfy regulatory requests the embryo would have to be contained so it did not come in direct contact with the liquid nitrogen. While this created a further complication, it also provided a huge opportunity to develop revolutionary IP that would significantly advance the industry. The IP we developed was in the form of a microfluidic pod which held the embryo safely in position while fluids could be transferred in and out of the pod. The pod could also be sealed, protecting the embryo from contact with the liquid nitrogen.
The current manual process involved an embryologist picking up an embryo on a small curved stick and running it through multi-steps of media formulation before dunking it directly into liquid nitrogen where the embryo could be stored for a period of time. While this manual process had major drawbacks, it had one advantage and that was that dropping an embryo directly in to liquid nitrogen achieved very fast freezing, or vitrification. By placing the embryo in the pod we had to undertake significant development to enable the sealed embryo to be vitrified at the required -10,000 degrees per second.
The consumable held the key
Over a series of months we finally arrived with a consumable pod design that successfully held the embryo in place over the course of minutes while we ran a series of media concentrations through it. By experimenting with materials and material thicknesses, we also achieved the required vitrification rate. By successfully developing the pod, which is effectively the core technology, we knew automation was now possible, even though at this stage we had not started to develop the instrument.
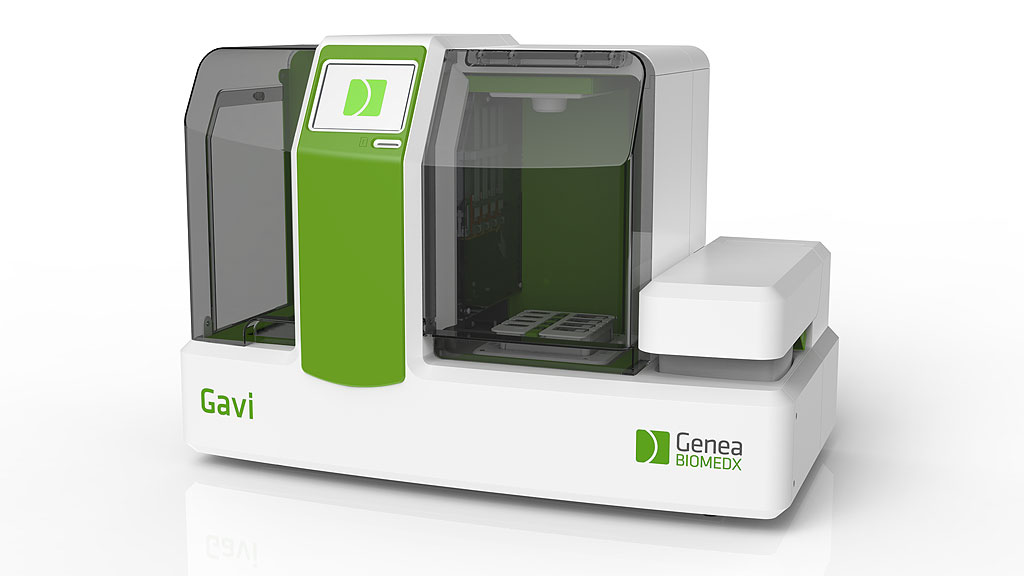
With the core technology issue solved, it was time to move on to developing an instrument that would automate the dispensing and aspirating of the media. We deliberately included a lot of touch points with potential customers through design. This involved many face-to-face interviews with potential users and we even set up an unbranded tradeshow stand at the world’s largest reproductive health conference to gain customer feedback on the human factors requirements. By the end of the conference we had a pretty good understanding of how that product was going to work in a lab, and it was now time to start developing the automated instrument which would go on to be known as Gavi (Genea Automated Vitrification Instrument).
While developing the instrument had its challenges, maintaining a strong market orientation throughout the development set us up for success. Over a period of approximately 18 months, using a series of prototypes and further rounds of customer trials, Gavi was completed and was part of the Genea Biomedx launch at the 2013 ESHRE conference in London.
Commercialization channels were developed in parallel with the technology
Throughout the product development process, Genea Biomedx and Planet Innovation had been developing sales, marketing and distribution channels for the instrument. We had also been working on early life manufacture so that we were able to scale up manufacture quickly after launch. This proactive approach to developing the commercialization strategy in parallel with the product dramatically increases the rate of early revenues.
My tips for anyone embarking on a similar journey are to prove that your core technology works, and works reliably, before you do you anything else. Secondly, build the instrument around user requirements that you continue to refine during development. And finally, ensure your commercialization strategy is planned well ahead of launch and covers everything from transfer to manufacture, marketing, service and sales distribution.
Gavi is the world’s first automated device for IVF vitrification – and it was achieved by starting with the end game in mind. It has changed the way IVF is performed by standardizing the way each embryo is handled and therefore increasing the fertility outcome for families around the world.